|
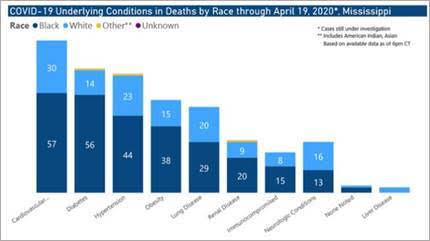
COVID-19 Health Equity Data: Race, ethnicity, age, gender and location data is needed to understand how COVID-19 is affecting our more vulnerable populations. In April, the Centers for Disease Control and Prevention started releasing nationwide data showing the race and ethnicity characteristics of COVID-19 cases, although race data was missing in 76% of cases. All states are now reporting some COVID-19 data, but the type and specificity of information that is collected varies considerably across states. Connecticut reports COVID-19 data by age, gender, race, ethnicity, at the town level and at nursing homes, but not at the zip code level or for health care workers. Just 12 states are reporting by race, ethnicity and zip code or census tract level. Currently, only Mississippi reports deaths broken down by both underlying conditions and race. See State Health and Value Strategies maps for more. Connecticut’s own Health Equity Solutions was featured in last week’s national SHSV webinar on tracking and taking action to address health disparities. Slides here; recording here. Health Equity Solutions has also published an article on Five Key Questions State Health Officials Can Ask Right Now to Advance Health Equity During COVID-19 Response Efforts and released the analysis of its recent survey and outreach effort to collect information about the impact of COVID-19 and measures to control its spread on underserved communities. UConn’s Health Disparities Institute is holding a Facebook Live conversation on racial profiling on Wednesday, May 13 at 3 PM with nationally renowned scholar activists, researchers, and policy advisors. DYK? Maryland Health Connection has an online Household Income Calculator to help applicants determine their Modified Adjusted Gross Income for the year in which they seek health coverage. How did other states do with their COVID-19 emergency enrollment periods?
How will COVID-19 impact insurers? A recent Wakely Consulting study says COVID-19 could cost US insurers anywhere between $56 billion to $556 billion through the next year. This report comes when health insurers are working on plans to determine their rates for the 2021 benefit year. A different study released in March by actuaries at Covered California estimated the cost of covering testing, treatment, and care for the 170 million Americans in the commercial market anywhere between $34 billion to $251 billion or more in the first year of the pandemic. The Wakely study was commissioned by America’s Health Insurance Plans (AHIP).
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |

 RSS Feed
RSS Feed